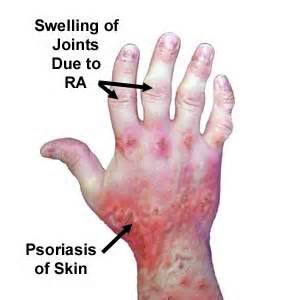
Arthritic Psoriasis: Diagnosis and Treatment of Psoriatic Arthritis
If you have arthritic psoriasis you know the pain and embarrassment that
can along with this disorder. This type of psoriasis not only is
painful on the outer layer of the skin, but within the joints as well.
If you have been diagnosed with this psoriatic arthritis, you may go through a series of emotions. You may wonder why and how you became afflicted with psoriasis and its related form of arthritis. You may wonder if there is anything that you can avoid in order to reduce the flareups.
Receiving a diagnosis of this disorder can cause many emotions. A supportive group may be able to help you sort through the feelings you experience with arthritic psoriasis.

Arthritic Psoriasis and the IMMUNE System
Understanding and Managing Psoriatic Arthritis
Psoriatic arthritis is a chronic inflammatory condition that affects both the skin and joints. It arises from a dysfunction in the immune system, which mistakenly attacks healthy tissues in the body, leading to inflammation and pain. This autoimmune response triggers both skin manifestations, characteristic of psoriasis, and joint inflammation, the hallmark of arthritis. The interplay of these two components makes psoriatic arthritis a complex condition requiring comprehensive management.
The Immune System's Role in Psoriatic Arthritis
At the core of psoriatic arthritis lies a malfunctioning immune system. Normally, the immune system acts as the body's defense mechanism, identifying and eliminating harmful invaders like bacteria and viruses. However, in individuals with psoriatic arthritis, this intricate system goes awry. Immune cells, specifically T cells, become overactive and mistakenly target the body's own tissues, particularly in the skin and joints. This misdirected immune response triggers a cascade of inflammatory processes, resulting in the characteristic symptoms of psoriatic arthritis. The inflammation manifests as redness, swelling, and pain in the affected joints and skin lesions.
Genetic Predisposition and Environmental Triggers
While the exact cause of psoriatic arthritis remains elusive, research suggests a strong genetic component. Individuals with a family history of psoriasis or psoriatic arthritis are at a significantly increased risk of developing the condition. Specific genes have been identified that contribute to this predisposition, although the complete genetic picture is still being unravelled. Environmental factors also play a role in triggering or exacerbating psoriatic arthritis. These triggers can vary from person to person and may include infections, stress, and certain medications. Identifying and managing these triggers can be crucial in controlling the disease's progression.
Coping with the Diagnosis and Managing Flare-Ups
Receiving a diagnosis of psoriatic arthritis can be overwhelming and confusing. Many individuals experience a range of emotions, including denial, fear, and uncertainty. Understanding the nature of the condition and its underlying causes can help alleviate some of these anxieties. Education about the disease process, treatment options, and self-management strategies is essential for empowering individuals to take control of their health.
Managing flare-ups, periods of increased disease activity, is a crucial aspect of living with psoriatic arthritis. Lifestyle modifications can play a significant role in minimizing the frequency and severity of these episodes. Limiting alcohol consumption and avoiding nicotine are important steps, as these substances can exacerbate inflammation. Maintaining a healthy weight can also reduce stress on the joints, alleviating pain and improving mobility. Protecting the skin from injury is essential, as skin trauma can trigger or worsen psoriatic lesions.
Seeking Support and Professional Guidance
Living with psoriatic arthritis can be challenging, but individuals do not have to face it alone. Support groups and online communities can provide valuable connections with others who understand the challenges of the condition. Sharing experiences, tips, and emotional support can make a significant difference in coping with the disease. Consulting with a rheumatologist, a specialist in arthritis and autoimmune diseases, is crucial for receiving appropriate medical care. The rheumatologist can develop a personalized treatment plan, which may include medications, physical therapy, and other interventions to manage symptoms and improve quality of life.
It's not easy to learn how the DISEASE may affect you.
Navigating the Emotional Landscape of a Psoriasis Diagnosis
The initial stages of a psoriasis diagnosis can be an emotionally turbulent time. Learning about the potential impact of this chronic skin condition on your life and making necessary adjustments to manage symptoms can feel overwhelming. It's essential to acknowledge these emotional challenges and seek support during this period.
Building a Support Network
Leaning on your family and friends during this time is crucial. Educating them about the struggles you face with psoriasis can foster understanding and empathy. Sharing your experiences with loved ones can provide comfort and alleviate feelings of isolation. Connecting with a support group of people also diagnosed with psoriasis can be immensely beneficial. Sharing experiences and coping strategies within a community of understanding individuals can empower you on your healing journey. Knowing that you're not alone in this experience can provide strength and encouragement.
Understanding Psoriasis and Taking Control
Psoriasis is an autoimmune disorder originating in the immune system. White blood cells, which normally protect the body against infection, become overactive and multiply rapidly. This immune dysfunction leads to the development of scaly, red patches on the skin, often accompanied by intense itching and pain. The unpredictable nature of psoriasis and its visible manifestations can contribute to feelings of confusion and frustration. Educating yourself about the disease, its triggers, and management strategies can help you regain a sense of control. Learning about ways to reduce psoriasis flare-ups can empower you to actively participate in your treatment and improve your quality of life.
Lifestyle Adjustments and Embracing a Positive Outlook
Making simple lifestyle changes can significantly impact your psoriasis symptoms. These changes may include adopting a healthy diet, managing stress levels, and avoiding known triggers. While navigating this emotional time, remember that psoriasis does not have to define or control your life. Focus on adapting your daily activities to accommodate your needs and prioritize self-care. Embrace a positive outlook and focus on the things you can control, such as seeking support, adhering to treatment plans, and making healthy lifestyle choices. By actively engaging in your own care and building a strong support system, you can navigate the challenges of psoriasis and live a fulfilling life.
 Psoriasis on the leg
Psoriasis on the legPágina de inicio
Mapa del sitio
Mapa del sitio en orden alfabético