Arthritis Psoriasis: What You Should Know about Psoratic Arthritis
 Does Psoriasis-Arthritis hurt?
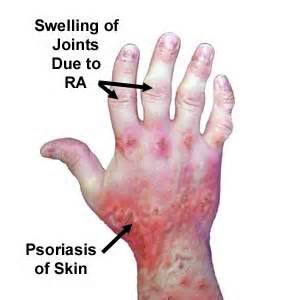
Does Psoriasis-Arthritis hurt?Arthritis Psoriasis is the type of psoriasis which causes pain in the joints. Psoriasis is caused when the white blood cells, called T-cells, overpopulate causing red scaly marks on the skin. Psoriasis can cause arthritis within the joints. Psoriasis can be treated through topical treatments or phototherapy.
Arthritis due to psoriasis can be diagnosed by an x-ray or laboratory work. Fortunately, there are many treatments for this type of arthritis.Psoriasis arthritis.
Diagnosing ARTHRITIS Psoriasis
Diagnosing Psoriatic Arthritis: A Comprehensive Guide
Psoriatic arthritis, a chronic inflammatory condition affecting joints, often presents diagnostic challenges due to its similarity to other forms of arthritis, particularly rheumatoid arthritis. A definitive diagnosis requires a combination of physical examination, medical history assessment, and specific laboratory and imaging tests. These tests not only help confirm the presence of psoriatic arthritis but also rule out other potential conditions, enabling a tailored treatment plan. Arthritis Psoriasis.
**Physical Examination and Medical History:**
The diagnostic journey typically begins with a thorough physical examination. Physicians carefully examine the affected joints, looking for signs of inflammation such as swelling, tenderness, redness, and limited range of motion. They also assess the skin and nails for characteristic psoriatic lesions, which can be a crucial clue in the diagnosis. A detailed medical history, including family history of psoriasis or psoriatic arthritis, is also essential.
**Imaging Techniques:**
Several imaging techniques play a vital role in visualizing the joint changes associated with psoriatic arthritis.
* **X-rays:** X-rays are often the initial imaging study performed. While they may not detect early changes in psoriatic arthritis, they can reveal characteristic features in more advanced cases. These include joint space narrowing, bone erosion, and bony outgrowths (osteophytes). X-rays are particularly useful in assessing the extent of joint damage and monitoring disease progression.
* **Magnetic Resonance Imaging (MRI):** MRI offers a more detailed view of both soft tissues (like tendons and ligaments) and bone. It is particularly sensitive in detecting early inflammatory changes in the joints and surrounding tissues, even before they become visible on X-rays. MRI is often used to evaluate specific areas like the spine and sacroiliac joints, which can be affected in psoriatic arthritis. It can also help differentiate psoriatic arthritis from other conditions like rheumatoid arthritis.
**Laboratory Tests:**
While there's no single blood test to definitively diagnose psoriatic arthritis, laboratory tests can help exclude other conditions and provide supporting evidence.
* **Rheumatoid Factor (RF):** This test detects the presence of rheumatoid factor, an antibody commonly found in rheumatoid arthritis. A negative RF test, while not conclusive, can help differentiate psoriatic arthritis from rheumatoid arthritis.
* **Joint Fluid Analysis:** In some cases, a physician may perform a joint aspiration, also known as arthrocentesis. During this procedure, a small amount of fluid is withdrawn from the affected joint using a needle. Analyzing the joint fluid can help identify uric acid crystals (indicative of gout) or exclude infections. While not specific to psoriatic arthritis, joint fluid analysis can provide valuable information about the inflammatory process.
* **Other Blood Tests:** Other blood tests, such as erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), can measure inflammation in the body. While elevated levels of these markers can suggest inflammation, they are not specific to psoriatic arthritis and can be elevated in various other conditions.
**Differential Diagnosis:**
Distinguishing psoriatic arthritis from other forms of arthritis, especially rheumatoid arthritis, is crucial for effective treatment. While both conditions can cause joint pain and inflammation, they differ in several key aspects. Rheumatoid arthritis typically affects the small joints of the hands and feet symmetrically, while psoriatic arthritis can affect a wider range of joints, including the spine and digits, often in an asymmetrical pattern. The presence of skin and nail changes, along with a negative rheumatoid factor test, further supports a diagnosis of psoriatic arthritis.
**Conclusion:**
Diagnosing psoriatic arthritis requires a comprehensive approach involving physical examination, medical history assessment, and a combination of imaging and laboratory tests. By carefully evaluating these factors, physicians can accurately diagnose psoriatic arthritis and differentiate it from other conditions, leading to appropriate and timely treatment.
Different types of MEDICATIONS
Understanding Psoriatic Arthritis: A Deeper Dive
Psoriatic arthritis, a chronic inflammatory condition, affects individuals with psoriasis, causing joint pain, stiffness, and swelling. Managing this condition effectively involves understanding its complexities and available treatment options. While this information provides a general overview, consulting with a rheumatologist is crucial for personalized diagnosis and treatment.
Medication Management for Psoriatic Arthritis
Several medications can help control the inflammation responsible for joint pain in psoriatic arthritis. However, it's essential to remember that not all medications are suitable for everyone, and a doctor must approve any medication before use. Self-treating can be risky and may lead to complications.
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
NSAIDs, such as ibuprofen (Advil, Motrin) and naproxen (Aleve), are commonly used to relieve pain and inflammation. These medications are often available over-the-counter, providing readily accessible relief. However, long-term NSAID use can have potential side effects, including gastrointestinal issues like ulcers and bleeding, kidney problems, and elevated blood pressure. Therefore, it's crucial to use NSAIDs judiciously and under a doctor's supervision, especially for extended periods.
Disease-Modifying Anti-Rheumatic Drugs (DMARDs)
DMARDs, unlike NSAIDs, work to slow the progression of psoriatic arthritis and reduce joint damage. These medications don't offer immediate relief; their effects become apparent gradually over time. While DMARDs can significantly improve long-term outcomes, they also carry potential side effects, including liver, lung, and kidney problems. Regular monitoring and open communication with your doctor are essential to manage these risks effectively.Arthritis Psoriasis.
Immunosuppressant Medications
In severe cases of psoriatic arthritis, immunosuppressants may be necessary to control the overactive immune system driving the inflammation. These medications are reserved for more aggressive cases due to their potential for serious side effects. Close monitoring by a healthcare professional is crucial when using immunosuppressants.
Tumor Necrosis Factor-Alpha (TNF-alpha) Inhibitors
TNF-alpha inhibitors represent another class of medications used in moderate to severe psoriatic arthritis. These drugs target a specific protein, TNF-alpha, which plays a key role in inflammation. While effective, TNF-alpha inhibitors can have serious side effects, emphasizing the importance of medical supervision.
Diagnosis and Treatment: A Collaborative Approach
Diagnosing psoriatic arthritis involves a combination of physical examination, medical history, and sometimes imaging studies or blood tests to rule out other conditions. Once diagnosed, treatment focuses on managing pain, controlling inflammation, and preventing joint damage. Your doctor will tailor the treatment plan to your specific needs, considering factors like disease severity, overall health, and potential medication side effects.
The Importance of Medical Guidance
While understanding the different medication options for psoriatic arthritis is helpful, it's paramount to remember that self-treating is strongly discouraged. All medications, including over-the-counter options, carry potential risks. Working closely with a healthcare professional is essential for safe and effective management of psoriatic arthritis. They can provide accurate diagnosis, recommend appropriate medications, monitor your progress, and adjust treatment as needed to minimize side effects and optimize outcomes.
Arthritis Psoriasis, my own Dead Sea experiences can help you
National Institute of Arthritis and Musculoskeletal and Skin Diseases
 Psoriasis on the leg
Psoriasis on the legPágina de inicio
Mapa del sitio
Mapa del sitio en orden alfabético